Part 4 of the 5-part Foot to Floor Series addressing how the feet and legs are related to the pelvic floor and potential causes of dysfunction. Fascia is more complex than any one blog post can describe, so here is a basic overview of how one of many chains can affect the pelvic floor or cause dysfunction.
What is fascia?
Fascia is the white stuff in a steak, the fibrous, supple, wonderful, nerve- conducting stuff that holds us all together. It travels throughout our bodies, everywhere we need mobile support.
therapists, 3rd ed. New York: Churchill Livingstone.
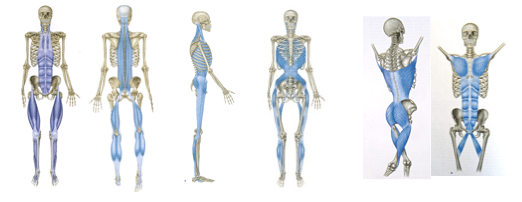
There are multiple “chains” in the body. The posterior fascia chain is the one I will reference most in this post, but it is fascinating how connected we are. We tend to think of bone and muscle, but fascia and it’s connectivity in the body is responsible for a significant amount of our mobility and support.
How does fascia relate to pelvic floor dysfunction?
If you look closely, you see how the fascia connects from the arch of the foot, up the calf, inner thigh, pelvic floor, back of the ribs, and neck to the throat. Tightness anywhere along this chain can present a problem. Like stated in the other blogs, the motion in the plantar fascia and toe is critical for hip extension and strong glueals. This helps with stability and support if you have incontience, prolapse, diastasis recti, and other pelvic dysfunctions.
Fascia also houses our nerves. Restrictions in fascia make nerves very unhappy. Many times nerve pain is actually a fascia restriction. Think of sciatica when you look at that fascia chain. I could have made nerves number 6 of the series as they leave the lumbar spine, down the leg and to the foot.
How do I know if my fascia is normal?
See a specialized pelvic health Physical Therapist. An orthopedic physical therapist can tell you about the legs and hips, but see a pelvic PT to address the fascia in the pelvic floor as well.
This fascia continues to connect to the pelvic organs including the bladder, uterus, and bowel. These organs need to remain mobile to slide past each other as they go about their business. Tightness can lead to decreased function and abdominal and pelvic pain.
Test yourself:
Bend to touch your toes and stop when you feel a gentle pull (anywhere). Where is that pull? We often think this is our hamstrings (and that may be true). However, notice if there is anything else. Do you feel a pull in the low back, SI joints, back of the knees, calves? If the head is gently hanging, you may feel it in the upper back or neck. This is what fascial tension can feel like. It is important to keep in hydrated and mobile throughout its length.
How does fascia get “tight”?
There are many ways fascia can lose mobility. For example, surgery, injury, poor nutrition, dehydration, age, or simply lack of use can all lead to less than optimal motion anywhere along the chain.
How is your breathing?
Fascia connects to our ribs, diaphragm, and throat. Therefore, lack of motion in these areas can restrict the ability to take a deep breath, and lack of regularly taking deep breaths can tighten the fascia.
Go ahead, take a deep breath. Your ribs should move. They should have some amount of motion all the way around to the back.
Looking at the post on diastasis recti (DRA) and prolapse, which are pressure problems, it’s easy to see that if we cannot control our breath, we cannot control our pressure. Imbalanced pressure and tightness from above is not helpful for incontinence and prolapse when the pelvic floor is weak and tight from below.
In conclusion:
Restriction, immobility and pain anywhere along any of our fascia connections can lead to as much, if not more, complications and pelvic floor dysfunction as the muscle and bone it surrounds. It is important to keep it all happy. If you aren’t sure how to get started, we are happy to help you locally, or contact us to help find a provider in your area.